Abstract
Background:
Inflammatory bowel disease (IBD) is a group of chronic inflammatory disorders of the gastrointestinal tract that affect approximately 70,000 children in the U.S. Anemia is the most common extra-intestinal symptom in children with IBD and is present in up to three-quarters of patients, most commonly due to iron deficiency.
Despite its prevalence and impact, iron deficiency remains undertreated in children with IBD. Oral iron supplementation is often considered inefficient for such patients due to intolerance, sub-optimal absorption, and the potential to worsen local disease inflammation within the gastrointestinal tract. In adults with IBD, intravenous (IV) iron is commonly used and capable of improving iron status even in the setting of persistent inflammation. Newer IV iron formulations with decreased dosing requirements and improved safety profiles have reduced barriers to its use in pediatric patients. However, minimal published data exist on the use of IV iron in pediatric IBD.
Objective:
To evaluate trends in diagnosis of iron deficiency and its management utilizing a large national children's hospital database in pediatric patients with IBD over a 5 year period. We hypothesized that the use of IV iron to treat iron deficiency anemia (IDA) would increase and receipt of blood transfusion would subsequently decrease over time.
Methods:
In this retrospective multicenter cohort study, we used the Pediatric Health Information System (PHIS) de-identified administrative database containing data from 48 not-for-profit tertiary care pediatric hospitals in the U.S. ICD-9 and ICD-10 codes for Crohn's disease and ulcerative colitis identified all inpatient admissions for IBD from January 2012 through December 2017. Diagnostic codes were also used to identify those patients with anemia or iron deficiency during their admission. Procedure codes were assessed for receipt of transfusions, and pharmaceutical billing codes were assessed for iron (intravenous and oral preparations). Data were analyzed descriptively.
Results:
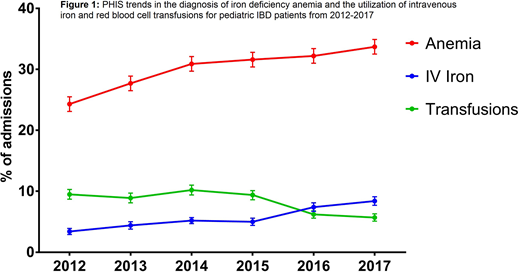
We identified 17,836 unique patients (9,308 male, 52.2%) with IBD diagnosis codes admitted between 2012 and 2017 for a total of 35,770 admissions. Median age at admission was 15.6 years (range 0 to 70 years; 733 (4.1%) > 21 years). There were 7,509 (42.1%) patients who also had a diagnosis of IDA during admission. Of the 35,770 admissions, iron therapy (oral or IV) was given in 7,918 admissions (22.1%). IV iron was given in 2,118 admissions (5.9%) and blood transfusions were given in 2,895 admissions (8.1%). Between 2012 and 2017, the prevalence of the diagnosis of IDA among IBD admissions increased from 24.3% in 2012 to 33.7% in 2017 (p<0.0001). Similarly, there was a steady increase in the proportion of IBD admissions that utilized IV iron, from 3.4% in 2012 to 8.4% in 2017 (p<0.0001). There was no difference in the use of oral iron over time (p=0.32). The proportion of admissions for IBD with red cell transfusions decreased over time from 9.5% to 5.7% (p<0.0001, Figure 1).
Discussion:
Iron deficiency anemia is highly prevalent among pediatric patients with IBD admitted to U.S. children's hospitals. The upward trend during this 5 year study period may potentially be due to increased recognition of this complication. Regarding management, we identified an increase in the use of IV iron for the treatment of IDA over time, and a decrease in admitted patients receiving transfusions. Further research is needed to further optimize detection of iron deficiency in pediatric IBD patients as well as evaluate the best approach for management of this common complication.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal